Clinical History
A 24-year-old female patient was recently diagnosed with hypoparathyroidism. She had a history of long-standing paraesthesia and muscle cramps in her distal extremities. She presented to us for MR imaging of brain following an episode of generalised tonic clonic seizure.
Imaging Findings
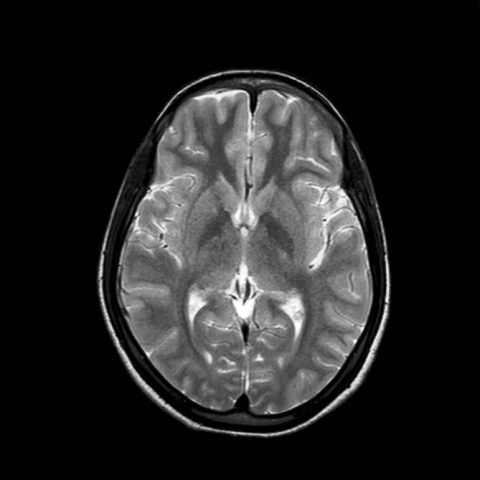
A 24-year-old female patient was recently diagnosed with hypoparathyroidism. She had history of long-standing paraesthesia and muscle cramps in her distal extremities. She presented to us for MR imaging of brain following an episode of generalised tonic clonic seizure. MR imaging of brain revealed symmetrical T1-hyperintensity of the bilateral basal ganglia, paraventricular region and dentate nuclei. Corresponding T2-weighted images revealed no overt signal intensity changes. On T2*GRE images these areas of signal alteration demonstrated hypointense signal. A CT was followed to confirm the findings which demonstrated symmetrical bilateral basal ganglia calcinosis.
Discussion
Hypoparathyroidism is an endocrinal disorder which occurs due to inadequate secretion or action of parathyroid hormone (PTH). Hypoparathyroidism can be either congenital or acquired. Its most common cause is iatrogenic typically following surgical excision or damage to the parathyroid glands during total thyroidectomy or radical neck dissection. PTH is secreted by the parathyroid glands and is the prime regulators of serum calcium concentration. Hypoparathyroidism results in loss of the direct as well as indirect effects of PTH on bone, the kidney, and the gut. Calcium and phosphate release from bone is impaired, calcium absorption from the gut is limited, calciuria develops despite hypocalcemia, and retention of phosphate from the urine causes increased plasma phosphate levels. The net effect is a decrease in serum calcium and an increase in serum phosphate. It is well known that this disturbed calcium and phosphorous metabolism may be associated with ectopic or metastatic calcium deposition in previously normal tissues such as lung, stomach, kidneys, and brain. Intracranial calcification in hypoparathyroidism has been well documented. Calcifications may be located at various sites in the cranium, but are particularly common in the basal ganglia. The most common site is the caudate nuclei, followed by the putamina, globus pallidi, thalamus, dentate nuclei, centrum semiovale and uncommonly the cerebral cortex. Although the exact aetiopathogenesis is not well understood, it is believed that microscopic colloid deposition around cerebral blood vessels is followed by calcification in the basal ganglia. Patients may remain asymptomatic or present with seizure disorders, extrapyramidal motor dysfunction or Parkinsonian features. Patients can also present with poor concentration, impaired memory, disorientation and apathy. Bilateral symmetrical calcification of the basal ganglia or more widespread intracranial structures can be easily detected on CT. Plain radiography has a limited role. Other entities which may demonstrate symmetrical basal ganglia calcification include metabolic disorders (Fahr disease), inflammatory conditions (toxoplasmosis, CMV), congenital or neurodevelopment diseases, carbon monoxide poisoning, hyperparathyroidism or following chemotherapy or radiotherapy. MR imaging is being increasingly used for evaluation of these patients. Basal ganglia calcification frequently demonstrates isointense to hypointense signal on T1- and T2-weighted images and T2* GRE images. However at times, calcification can appear hyperintense on T1-weighted images as is seen in the present case. T1-shortening is believed to relate to the varying crystalline structure of the calcification. Calcium particles with greater surface area are believed to show greater T1-relaxation. A similar pattern of symmetrically hyperintense basal ganglia on T1-weighted images may be seen in hepato-cerebral degeneration, Wilson’s disease, and in those taking parentral nutrition.
Differential Diagnosis List
Extensive basal ganglia calcification related to hypoparathyroidism
Final Diagnosis
Extensive basal ganglia calcification related to hypoparathyroidism