Rare jaundice cause in diabetic patient
SectionAbdominal imaging
Case TypeClinical Cases
Authors
Federica Fiocchi, Marco Ferrrari, Grazia Amorico, Pietro Torricelli
Patient74 years, male
A diabetic male patient (74-year-old) was admitted to emergency department with obstructive jaundice and weight loss. Previous clinical history was silent. Blood work-up showed total bilirubin 6.7 mg/dl, GPT 742 U/L, amylase 147 U/L and lipase 431 U/L.
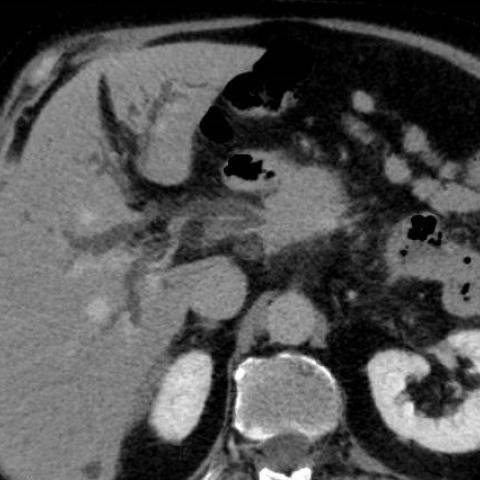
Abdominal ultrasound was performed to evaluate pancreatic region and biliary system and it revealed hypoechoic area within the pancreas head associated with common and intrahepatic bile ducts dilatation. The diameter of the common bile duct was 1,15cm. No ascites neither abdominal masses were found. CT scan was performed and showed diffuse enlargement of the whole pancreas with homogeneous contrast-enhancement, sausage-like appearance and tail retraction. Pancreatic duct was regular, non-dilated, but there was minimal peripancreatic stranding and mainly a capsule-like low-attenuation rim. The biliary system was dilated with thickened and enhanced walls; moreover the intrapancreatic tract was narrowed with upstream dilation. Small peripancreatic and retroperitoneal lymph nodes were associated. These findings suggested several differential diagnosis: pancreatic ductal adenocarcinoma, pancreatic lymphoma, acute pancreatitis and autoimmune pancreatitis (AIP). The biopsy, serology and the response to steroid therapy confirmed the diagnosis of autoimmune pancreatitis.
Incidence of autoimmune pancreatitis is unexplored, reported about 2-11% of all cases of chronic pancreatitis and 2-6% cases of pancreatic resection for suspected cancer. Mean age of patients is 60 years with male-to-female ratio of 15:2. Clinical features are aspecific: weight loss, obstructive jaundice, generic abdominal pain and diabetes mellitus. [1,4,6]
AIP is classified into type I and type II. Type I, AIP lymphoplasmacytic sclerosing pancreatitis, is a related IgG4 systemic disease without granulocyte epithelial lesions at hystology. Type II, chronic duct-centric idiopathic pancreatitis, reveals a predilection for young patients, in 30% of cases it is associated with inflammatory bowel disease and granulocyte epithelial lesions, but not related to IgG4 diseases. [1]
There are three imaging pathological patterns of AIP: diffuse, focal or multifocal. [1,3,4,6] The diffuse pattern, as the presented case, is the most common: sausage-like enlargement, with loss lobular contours, lack of pancreatic clefts and hypodense capsule-like peripheral rim (12-40%) that represents fluid and fibrous tissue due to an inflammation process. The focal pattern shows a lesion within the pancreatic head with absent, or just mild, dilation of the main pancreatic duct. The multifocal pattern is the less common. [1,4,6]
The International Consensus Diagnostic Criteria for Autoimmune Pancreatitis requires: imaging, serology, other organ involvement, pancreatic histology and response to steroid therapy (optional criterion). [1,2] Most common extra-pancreatic manifestations include: pseudo-inflammatory kidney’s disease, cholangitis, diffuse lymph-adenopathy, retroperitoneal fibrosis, swelling of the salivary glands. [4]
The patient started corticosteroid therapy, and after five months CT scan demonstrated gradual global improvement of pancreatic swelling with disappearance of sausage-like morphology associated to serology betterment. [5]
Regarding the present case, radiologic and histological features, positive serology and suboptimal response to steroid therapy suggested the diagnosis of a Type I AIP.
Apart from AIP, other differential diagnosis include ductal adenocarcinoma, pancreatic lymphoma and acute oedematous pancreatitis. Some CT findings, typically seen in ductal adenocarcinoma, are absent in AIP such as significant dilation of a segment of the main pancreatic duct followed by an abrupt narrowing, atrophy of the parenchyma and involvement of the major peripancreatic vessels. [1,6] (Fig.6) Primary pancreatic lymphoma is commonly a B-cell subtype. Imaging diagnosis is based mainly on ancillary findings, such as retroperitoneal-pelvic enlarged lymph nodes and splenic lesions with just a mild biliary or pancreatic ductal obstruction.[7,8] (Fig.7) The diffuse enlargement and mild peripancreatic stranding can mimic a mild oedematous pancreatitis. [6] (Fig.8) Clinical and laboratory features suggest the differential diagnosis.
Written informed patient consent for publication has been obtained.
[1] S.Crosara, M.D’Onofrio Riccardo De Robertis, Emanuele Demozzi, Stefano Canestrini, Giulia Zamboni, Roberto Pozzi Mucelli (2014) Autoimmune pancreatitis: multimodality non-invasive imaging diagnosis World J Gastroenterol. 7; 20(45): 16881–16890 (PMID: 25493001)
[2] Shimosegawa T, Chari ST, Frulloni L, Kamisawa T, Kawa S, Mino-Kenudson M, Kim MH, Kloppel G, Lerch MM, Lohr M, Notohara K, Okazaki K, Schneider A, Zhang L (2011) International Consensus Diagnostic Criteria for autoimmune Pancreatitis: guidelines of International Association of Pancreatology International Association of Pancreatology. Pancreas. 40(3):352-8. (PMID: 21412117)
[3] Kiran K Busireddy, Mamdoh AlObaidy, Miguel Ramalho, Janaka Kalubowila, Liu Baodong, Ilaria Santagostino, and Richard C Semelka (2014) Pancreatitis imaging approach World J Gastrointestinal Pathophysiology. 15; 5(3): 252-270 (PMID: 25133027)
[4] Paraskevi A. Vlachou, Korosh Khalili, Hyun-Jung Jang, Sandra Fischer, Gideon M. Hirschfield, Tae Kyoung Kim (2011) IgG4-related Sclerosing Disease: Autoimmune Pancreatitis and Extrapancreatic Manifestation RadioGraphics 31(5): 1379-402 (PMID: 21918050)
[5] Dushyant V. Sahani, Nisha I. Sainani, Vikram Deshpande, Mehrine S. Shaikh, Dmitry L. Frinkelberg, Carlos Fernandez–del Castillo (2009) Autoimmune pancreatitis disease evolution, staging, response assessmet, and CT features the predict response to corticosterioid therapy Radiology 250:118-129 (PMID: 19017924)
[6] Satomi Kawamoto, Stanley S. Siegelman, Ralph H. Hruban, Elliot K. Fishman (2008) Lymphoplasmacytic Sclerosing Pancreatitis (Autoimmune Pancreatitis): evaluation with mutidetector CT RadioGraphics 28:157-70 (PMID: 18203936)
[7] Maria A. Manning, Edina E. Paal, Amogh Srivastava, Koenraad J. Mortele (2018) Nonepithelial Neoplasms of the Pancreas, Part 2: Malignant Tumors and tumors of uncertain malignant potential RadioGraphics 38(4):1047-1072 (PMID: 29787363)
[8] Gavin Low, Anukul Panu, Noam Millo, Edward Leen (2011) Multimodality Imaging of Neoplastic a Non-neoplastic Solid Lesions of the pancreas RadioGraphics 31(4):993–1015 (PMID: 21768235)
| URL: | https://www.eurorad.org/case/16542 |
| DOI: | 10.35100/eurorad/case.16542 |
| ISSN: | 1563-4086 |
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.