Abdominal aortic aneurysm associated with antiphospholipid syndrome: Imaging findings
SectionCardiovascular
Case TypeClinical Cases
Authors
Alberto Martínez-Martínez, Eduardo Ruiz-Carazo, Jade García-Espinosa
Patient36 years, female
A 36-year-old female patient had been diagnosed with antiphospholipid syndrome (APS) at the age of 27 with detection of antiphospholipid antibodies in the serum. At that time, antinuclear antibodies were repeatedly negative. She came to our Emergency Department with fever and pain in the lower dorsal region and epigastrium.
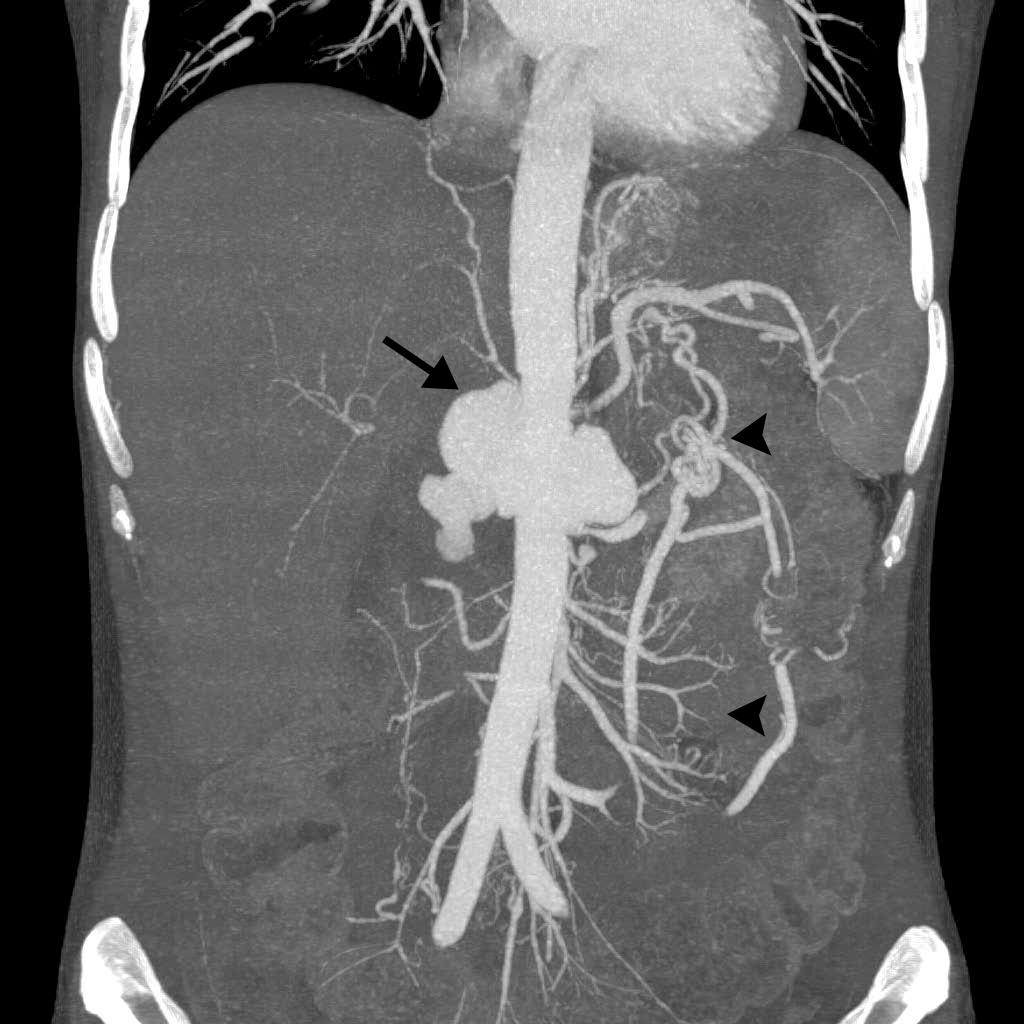
Multidetector computed tomography (MDCT) revealed a large polylobulated saccular aneurysm of the abdominal aorta cranial to the renal arteries, with a maximum diameter of 7 cm (Fig. 1). It was surrounded by a thick and irregular wall of inflammatory appearance that showed moderate enhancement after intravenous contrast material (IVC) administration (Fig. 2). Infiltration of neighbouring tissues and vascular structures was observed, with total occlusion of the coeliac trunk and superior mesenteric artery (arrow and arrowhead in figure 3). Both arteries were recanalised distally via collaterals that mainly arose from the inferior mesenteric artery (arrow in Fig. 4). The right renal artery was also infiltrated, showing almost total obstruction, with a major reduction in right kidney size and poor enhancement of the right versus left renal parenchyma. There was no sign of atherosclerotic involvement of the aorta or of other abdominal arteries.
APS is a clinical condition characterised by recurrent fetal loss, venous and/or arterial thrombosis, and thrombocytopenia associated with elevated antiphospholipid antibody titers [1]. APS was originally reported in patients with systemic lupus erythematosus (SLE) but has more recently been considered an independent syndrome (primary APS) [2]. There are few examples in the literature of an association between APS and onset of abdominal aortic aneurysm [3], and none showed imaging studies of the aneurysm with the marked inflammatory characteristics observed in the present case, which simulated an infectious or mycotic aneurysm [4]. However, it was not clearly demonstrated to be secondary to vasculitis. The coexistence of arterial aneurysms and APS creates a therapeutic dilemma, because the latter must be treated by anticoagulation, which may favour aneurysm bleeding.
The present patient was initially diagnosed with primary APS, developing SLE with renal involvement eight years later. Abdominal aortic aneurysm was clinically manifest at around six months after the SLE diagnosis. Hence, we consider the aneurysm to have been associated with the APS and not with the SLE. Aneurysms related to a primary APS have been reported in splenic, hepatic, and renal arteries [5], pancreatic, renal, and superior mesenteric arteries [6], pulmonary arteries [7], coeliac trunk and superior mesenteric, splenic, renal, and iliac arteries [8], and hepatic artery [9]. In 2008, Szyper-Kravitz et al. [3] described four patients with abdominal aortic aneurysm associated with primary APS, although images were only shown of two of the cases. Our radiological study revealed a large aneurysm with saccular polylobulated morphology and no evidence of mural thrombus or calcification. Only one of the aortic abdominal aneurysms reported by Szyper-Kravitz et al. was saccular, while the remaining cases were fusiform. In contrast, the visceral aneurysms reported in patients with APS were all saccular [5-9]. A unique feature of the aneurysm in the present patient was its “inflammatory” appearance, with replacement of the aortic wall by a thick and irregular wall and the infiltration and destruction of the walls of neighbouring arterial vessels. This behaviour has not been reported in any of the cases consulted. It is highly unlikely that atherosclerosis was responsible for the aneurysm in the present case, given that no signs of this disease were detected in the abdominal aorta not affected by the aneurysm or in the abdominal arteries.
The pathology report revealed absence of vasculitis. Mycotic aneurysm was ruled out by running the appropriate tests.
Written informed patient consent for publication has been obtained.
[1] Hughes GR (1983) Thrombosis, abortion, cerebral disease and lupus anticoagulant. Br Med J (Clin Res Ed) 287: 1088-9 (PMID: 6414579)
[2] Asherson RA, Khamashta MA, Ordi-Ros J, Derksen RH, Machin SJ, Barquinero J et al. (1989) The “primary” antiphospholipid syndrome: major clinical and serological features. Medicine (Baltimore) 68: 366-74 (PMID: 2509856)
[3] Szyper-Kravitz M, Altman A, de Carvalho JF, Bellisai F, Galeazzi M , Eshet Y et al. (2008) Coexistence of the Antiphospholipid Syndrome and Abdominal Aortic Aneurysm. Isr Med Assoc J 10: 48-51 (PMID: 18300573)
[4] Kurata A, Kawakami T, Sato J, Sakamoto A, Muramatsu T, Nakabayashi K (2011) Aortic aneurysms in systemic lupus erythematosus: a meta-analysis of 35 cases in the literature and two different pathogeneses. Cardiovasc Pathol 20 (1): 1-7 (PMID: 20133169)
[5] Koutoulidis V, Chatziioannou A, Kostopoulos C, Kontogiannis S, Skiadas V, Mourikis D et al (2005) Primary antiphospholipid syndrome: a unique presentation with multiple visceral aneurysms. Ann Rheum Dis 64: 1793-4 (PMID: 16284347)
[6] Dongola A, Foord KD (2000) Angiographic features associated with antiphospholipid syndrome. Br J Radiol 73: 1215-8 (PMID: 11144802)
[7] Chung MH, Lee HG, Kwon SS, Kim YS, Park SH (2002) Pulmonary arterial aneurysms in primary antiphospholipid antibody syndrome. J Comput Assist Tomogr 26: 608-12 (PMID: 12218828)
[8] Ehtuish EF, Mishra A (2008) Multiple visceral aneurysms in antiphospholipid antibody syndrome- an unusual presentation. Br J Radiol 81: e184-7 (PMID: 18559896)
[9] Vancheri F, Dovico R, Croce E, Di Falco G (2007) Hepatic artery aneurysm rupture in a woman with primary antiphospholipid syndrome. Lupus 16: 355-7 (PMID: 17576738)
| URL: | https://www.eurorad.org/case/16406 |
| DOI: | 10.35100/eurorad/case.16406 |
| ISSN: | 1563-4086 |
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.