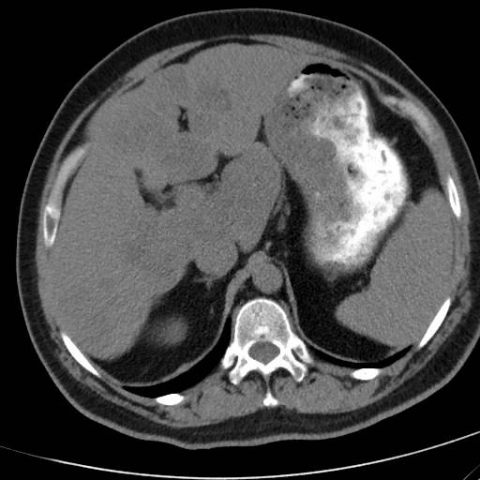
Axial NECT and CECT images of liver sarcoidosis



Abdominal imaging
Case TypeClinical Cases
AuthorsGalateia Skouroumouni, Charikleia Mauridou, Despina Panagiotidou, Melpomeni Kosmidou, Stavroula Pervana, Sofia Papaioannou
Patient35 years, male
[1] Newman LS, Rose CS, Maier LA. (1997) Sarcoidosis. N Engl J Med 336:1224-1234 (PMID: 9110911)
[2] Ayyala US, Padilla ML. (2006) Diagnosis and treatment of hepatic sarcoidosis. Curr Treat Option Gastroenterol 9(6):475-483 (PMID: 17081481)
[3] Blich M, Edoute Y. (2004) Clinical manifestations of sarcoid liver disease. J Gastroenterol Hepatol 19(7): 732-737 (PMID: 15209617)
[4] Cremers J, Drent M, Driessen A, et al. (2012) Liver-test abnormalities in sarcoidosis. Eur J Gastroenterol Hepatol 24(1):17-24 (PMID: 22008629)
[5] Hoeffel C, Bokemeyer C, Hoeffel JC, Gaucher H, Galanski M, Fomes P. (1996) CT hepatic and splenic appearances with sarcoidosis. Eur J Radiol 23: 94-96 (PMID: 8886715)
[6] Warshauer DM, Molina PL, Hamman SM, et al. (1995) Nodular sarcoidosis of the liver and spleen: analysis of 32 cases. Radiology 195(3): 757-762 (PMID: 7754007)
[7] Koyama T, Ueda H, Togashi K, Umeoka S, Kataoka M, Nagai S. (2004) Radiologic manifestations of sarcoidosis in various organs. Radiographics 24(1):87-104 (PMID: 14730039)
[8] Palmucci S, Torrisi SE, Caltabiano DC, et al. (2016) Clinical and radiological features of ectra-pulmonary sarcoidosis: a pictorial essay. Insights Imaging 7(4): 571-587 (PMID: 27222055)
| URL: | https://www.eurorad.org/case/15636 |
| DOI: | 10.1594/EURORAD/CASE.15636 |
| ISSN: | 1563-4086 |
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.