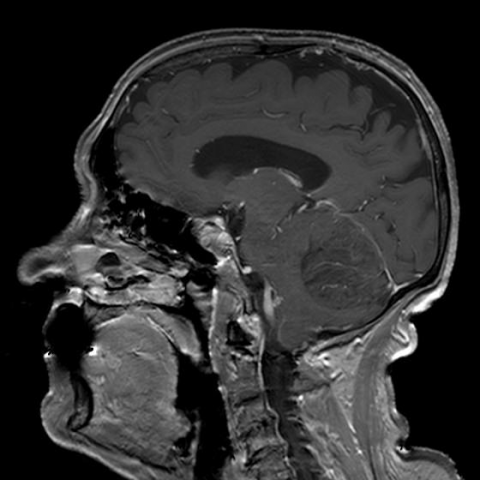
T2W/FLAIR images of dysplastic gangliocytoma
Dysplastic gangliocytoma of the cerebellum in an elderly patient: MR-imaging
SectionNeuroradiology
Case TypeClinical Cases
AuthorsKaterina Manavi, Galateia Skouroumouni, Filippos Sarafis, Giannis Petmezaris, Eliza Stavride, Ioannis Tsitouridis
Patient77 years, female
LDD is characterised by progressive enlargement of the cerebellar cortex. [4] The histological findings typically show non-neoplastic tissue consisting of cerebellar folia occupied by hypertrophic neurons of the internal granule cell layer. [5] The outer layer is dominated by hypermyelinated axons from abnormal ganglion cells. Mitosis and proliferation are absent, and Purkinje cells and white matter are diminished.
Clinical symptoms are caused by gradual increase of intracranial pressure (mass effect/secondary obstructive hydrocephalus), and cerebellar dysfunction. Most patients complain of slowly aggravating symptoms: occipital headache, vertigo, cranial nerve palsies, and cerebellar ataxia. The duration of symptoms ranges from few months to more than 10 years. [6] Abrupt deterioration of the previously vague neurological complaints may indicate acute herniation and imminent death. [2]
MRI allows recognition of the cortical nature of the lesion and preservation of the gyral pattern. [6] A mass is detected in the posterior fossa, commonly appearing with a striated pattern of hypointensity on T1WI and hyperintensity on T2WI alternating with isointense bands of tissue. The atrophic white matter, the adjacent layers of abnormal ganglionic neurons and the innermost part of the molecular layers appear hypointense on T1WI and hyperintense on T2WI/FLAIR. The outer part of the molecular layer of adjacent folia and the intervening leptomeningeal space are isointense to normal cerebellar tissue both on T1WI and T2WI. [4, 5, 7]
The disease is typically unilateral, with a predilection for the left cerebellar hemisphere. [2] The LDD lesions may show a very mild or no enhancement, which indicates that there is no significant disturbance of the blood-brain barrier. [6] If enhancement is present, other diagnoses, such as haemangioblastoma, might be suggested. [6, 7] The affected cerebellar hemisphere is usually asymmetrically widened. [2] Depending on the size of the lesion, mass effect with displacement of the fourth ventricle and obstructive hydrocephalus may occur. [1, 8] Diffusion MR shows a hyperintense area at the level of the lesion, due to T2 shine through effect. [5, 9] In the ADC map, the mass appears isointense to the cerebellar parenchyma, since the percentage of free water does not vary. The "tiger-striped" pattern of enlarged cerebellar folia is pathognomonic of LDD. [1, 2, 4-9] MRI associated with DWI provides a definite diagnosis of the disease. [9]
[1] Hariri OR, Khachekian A, Muilli D, et al. (2013) Acute-onset cerebellar symptoms in Lhermitte-Duclos disease: case report. Cerebellum 12(1):127-30 (PMID: 22692559)
[2] Ozeren E, Gurses L, Mehmet S, Er U, Önder E, Arıkök AT (2014) L'hermitte-Duclos disease in an elderly patient: a case report and review of the review of the literature. Asian J Neurosurg 9(4):246 (PMID: 25685239)
[3] Yağci-Küpeli B, Oguz KK, Bilen MA, Yalçin B, Akalan N, Büyükpamukçu M. (2010) An unusual cause of posterior fossa mass: Lhermitte-Duclos disease. J Neurol Sci 290(1-2):138-41 (PMID: 20060133)
[4] Williams LG, Brimage P, Lechner C, Taylor RL, Masters L, Welgampola MS (2014) Lhermitte-Duclos disease presenting with atypical positional nystagmus. J Clin Neurosci 21(9):1647-9 (PMID: 24842320)
[5] Inoue T, Nishimura S, Hayashi N, Numagami Y, Kaimori M, Nishijima M (2007) Ectopic recurrence of dysplastic gangliocytoma of the cerebellum (Lhermitte-Duclos disease): a case report. Brain Tumor Pathol 24(1):25-9 (PMID: 18095141)
[6] Anik Y, Anik I, Koc K, Inan N, Akansel G, Demirci A (2007) MR Spectroscopy findings in Lhermitte-Duclos disease. A case report. Neuroradiol J 20(3):278-81 (PMID: 24299666)
[7] Sen KK, Gunasekaran K, Kanagaraj V (2013) Imaging in Lhermitte: Duclos disease. South Asian J Cancer 2(3):131 (PMID: 24455585)
[8] . Yang MS, Kim CH, Cheong JH, Kim JM (2012) Lhermitte-Duclos disease presenting with hydrocephalus. Acta Neurochir Suppl 113:161-5 (PMID: 22116444)
[9] Giorgianni A, Pellegrino C, De Benedictis A, et al. (2013) Lhermitte-Duclos disease. A case report. Neuroradiol J 26(6):655-60 (PMID: 24355184)
| URL: | https://www.eurorad.org/case/14955 |
| DOI: | 10.1594/EURORAD/CASE.14955 |
| ISSN: | 1563-4086 |
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.