Clinical History
A 36-year-old female patient presented with a history of epigastric pain and nausea on-and-off for 6 months. There was no history of vomiting/loose stools/fever. There however was a history of laproscopic cholecystectomy 4 years before. Lab results showed evidence of obstructive jaundice.
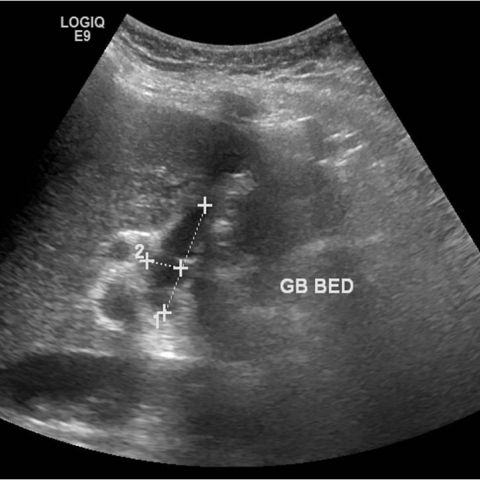
Imaging Findings
On ultrasound (US) abdomen, a minimal intrahepatic biliary tract dilatation (IHBRD) was seen. A well-defined elliptical cystic lesion of 32x10mm in size was seen in GB fossa, communicating with CHD down - likely to be a cystic duct remnant. No internal echoes/ calculi were noted within. No free fluid was seen around. The CBD was mildly dilated, measuring 12mm. A 5mm isoechoic focus with no posterior acoustic shadow representing sludge ball/ calculus was seen in CBD. The CBD distal end was seen tapering normally. Pancreatic duct was not dilated.
The CECT abdomen showed minimal IHBRD, dilated cystic duct remnant (45x12mm), related to dilated CHD (12mm) laterally, spiralling around it and showing lower insertion postero-medially forming the dilated CBD (14mm). No calculi were noted in cystic duct remnant/CBD. No abnormal contrast enhancement was seen in liver/cystic duct remnant.
MRCP confirmed the findings on US & CECT and also showed a 5mm calculus in distal CBD. The ampulla appeared normal.
Discussion
When a patient in status post cholecystectomy develops symptoms that are similar to the pre-cholecystectomy state such as right hypochondrial pain, dyspepsia and jaundice, it is called post cholecystectomy syndrome (PCS). Womack and Crider first described PCS in 1947. Incidence is found to be as high as 40% in one study, with a female preponderance. Patients can develop this syndrome in an early or late post-operative period [1, 2].
Most common aetiology of this syndrome is of extrabiliary origin like reflux esophagitis, acid peptic disease and chronic pancreatitis. Out of the biliary causes, most common causes in early onset include biliary tract injury, dropped/residual/recurrent calculi, and in late onset include dilated remnant cystic duct, CBD stricture, sphincter of oddi stricture or dysfunction [1, 2].
Radiologically PCS evaluation starts with US abdomen and if it is inconclusive followed by MRCP which has overcome the CT in hepatobiliary evaluation. MRCP is a non-invasive and reliable alternative method to direct cholangiography which is considered as a gold standard investigation [3, 4].
Bile tract injury can present as biliary obstruction if the injury is mild and as bile leakage if it is severe [1]. Calculi, either in the cystic duct remnant or CBD are considered residual if they are found within two years of the post-operative period and considered as recurrent if found after two years [3]. Calculi are seen as an echogenic structure with posterior acoustic shadowing if the size is large on US, hyperdense foci on CT and smooth hypointense filling defect with a surrounding rim of hyperintense bile on MRCP [3]. MRCP has high sensitivity and specificity in finding the biliary calculi. Dropped/ slipped calculi are commonly seen in an intrahepatic/sub-diaphragmatic location/in peritoneum or parietal wall with or without surrounding abscess formation [2, 3].
Cystic duct remnant is considered dilated if it measures > 4mm in diameter and > 2cm in length. It can present with or without evidence of inflammation and/or calculi within [3]. Sphincter of oddi dysfunction is evaluated with manometry. Other investigations employed are dynamic hepatobiliary scintigraphy with Tc-99M called DISIDA or HIDA scans [2, 3].
PCS is managed based on the aetiology. Medical treatment is usually enough to treat non-biliary causes. For biliary causes, usually laparoscopic cystic duct remnant resection, endoscopic sphincterotomy, sphincteroplasty, or stone removal are done. In very few patients not responding to these procedures only need laparotomy [5]. Most of the causes of PCS are treatable and imaging plays a major role in the diagnosis and treatment plan of PCS.
Differential Diagnosis List
Post cholecystectomy syndrome secondary to dilated cystic duct remnant and recurrent CBD calculi.
CBD/ampulla stricture
Biliary dyskinesia
Final Diagnosis
Post cholecystectomy syndrome secondary to dilated cystic duct remnant and recurrent CBD calculi.