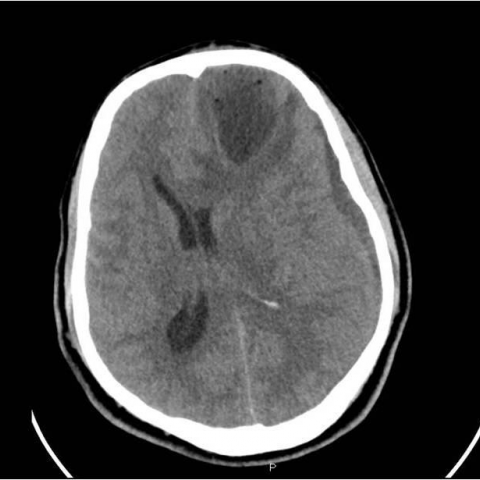
Brain Abscess Pre-operative Plain CT



Neuroradiology
Case TypeClinical Cases
AuthorsMuhammad Asim Rana, Ahmed F. Mady, Abdulrehman Alharthy, Omar E. Ramadan, Waleed T. Hashim, Sameh A. Ashmawi, Mohammed A. Alodat, Mahmoud H. AlKurdi, Mohammed M. Gharba, Ahmed Ragab, Mazen A. Hallak
Patient37 years, male
[1] Chun CH, Johnson JD, Hofstetter M, Raff MJ (1986) Brain abscess. A study of 45 consecutive cases. Medicine (Baltimore) 65(6):415. (PMID: 3784900)
[2] Bakshi R, Wright PD, Kinkel PR, Bates VE, Mechtler LL, Kamran S, Pullicino PM, Sirotkin I, Kinkel WR (1999) Cranial magnetic resonance imaging findings in bacterial endocarditis: the neuroimaging spectrum of septic brain embolization demonstrated in twelve patients. J Neuroimaging 9(2):78 (PMID: 10208104)
[3] Gallagher RM, Gross CW, Phillips CD (1998) Suppurative intracranial complications of sinusitis. Laryngoscope 108(11 Pt 1):1635. (PMID: 9818818)
[4] Kangsanarak J, Fooanant S, Ruckphaopunt K, Navacharoen N, Teotrakul S (1993) Extracranial and intracranial complications of suppurative otitis media. Report of 102 cases. J Laryngol Otol 107(11):999. (PMID: 8288994)
[5] Patel KS, Marks PV (1989) Multiple brain abscesses secondary to bronchiectasis. A case of 34 discrete abscesses in one brain. Clin Neurol Neurosurg 91(3):265. (PMID: 2548794)
[6] Schlaeffer F, Riesenberg K, Mikolich D, Sikuler E, Niv Y (1996) Serious bacterial infections after endoscopic procedures. Arch Intern Med 156(5):572. (PMID: 8604964)
[7] Staecker H, Nadol JB Jr, Ojeman R, McKenna MJ (1999) Delayed intracranial abscess after acoustic neuroma surgery: a report of two cases. Am J Otol 20(3):369. (PMID: 10337980)
[8] Nielsen H, Gyldensted C, Harmsen A (1982) Cerebral abscess. Aetiology and pathogenesis, symptoms, diagnosis and treatment. A review of 200 cases from 1935-1976. Acta Neurol Scand 65(6):609. (PMID: 7113666)
[9] Lakshmi V, Rao RR, Dinakar I (1993) Bacteriology of brain abscess--observations on 50 cases. J Med Microbiol 38(3):187. (PMID: 7681113)
[10] Brook I (1992) Aerobic and anaerobic bacteriology of intracranial abscesses. Pediatr Neurol 8(3):210. (PMID: 1622518)
[11] Guppy KH, Thomas C, Thomas K, Anderson D (1998) Cerebral fungal infections in the immunocompromised host: a literature review and a new pathogen--Chaetomium atrobrunneum: case report. Neurosurgery 43(6):1463. (PMID: 9848862)
[12] Britt RH, Enzmann DR (1983) Clinical stages of human brain abscesses on serial CT scans after contrast infusion. Computerized tomographic, neuropathological, and clinical correlations. J Neurosurg 59(6):972. (PMID: 6631519)
[13] Leuthardt EC, Wippold FJ 2nd, Oswood MC, Rich KM (2002) Diffusion-weighted MR imaging in the preoperative assessment of brain abscesses. Surg Neurol 58(6):395. (PMID: 12517619)
[14] Mathisen GE, Johnson JP (1997) Brain abscess. Clin Infect Dis 25(4):763. (PMID: 9356788)
[15] Cavuşoglu H, Kaya RA, Türkmenoglu ON, Colak I, Aydin Y (2008) Brain abscess: analysis of results in a series of 51 patients with a combined surgical and medical approach during an 11-year period. Neurosurg Focus 24(6):E9. (PMID: 18518754)
[16] Brouwer MC, Coutinho JM, van de Beek D (2014) Clinical characteristics and outcome of brain abscess: Systematic review and meta-analysis. Neurology 82(9):806-13. (PMID: 24477107)
| URL: | https://www.eurorad.org/case/11786 |
| DOI: | 10.1594/EURORAD/CASE.11786 |
| ISSN: | 1563-4086 |