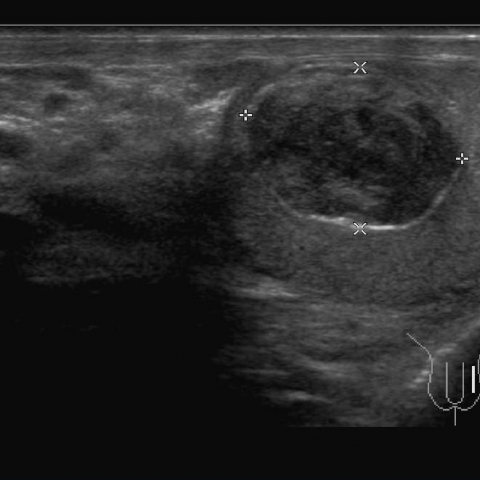
Left testicular epidermoid cyst
Epidermoid cyst - left testicular benign mass
SectionUroradiology & genital male imaging
Case TypeClinical Cases
AuthorsUmair Riaz Ahmad1, Jie Li1 , Shagufta Jabeen2, Liu Yan1, Ning Song1
Patient27 years, male
Ultrasound features were highly suggestive of benign nature of the mass. Serum α-feto protein & β–HCG levels were well within normal limits. Histopathology sections proved the benign nature of the lesion and ascertained it to be an epidermoid cyst. Patient was offered testis sparing surgery with partial orchidectomy. He recovered un-eventfully.
The scrotal masses can be classified as: Testicular & extra-testicular.
A) Testicular masses can further be divided into mainly solid – germ cell tumour, stromal cell tumour, lymphoma, leukaemia, metastasis from prostate, lung, melanoma, renal, and GIT, carcinoid, tuberculosis, abscess, inflammatory pseudotumour, haematoma, focal orchitis, sarcoidosis and rare cystic testicular masses – tubular ectasia of the rete testis, cystic dysplasia of the rete testis, non-neoplastic cysts including tunica albuginea cyst, intratesticular cyst, dermoid cyst, epidermoid cyst, benign/mature cystic teratoma, cystic lymphangioma, serous papillary cystic tumour, cystadenoma / adenofibroma of the rete testis, intratesticular spermatocele, intratesticular varicocele, haemorrhage, infarction, and necrosis.
B) The most common extra-testicular scrotal masses are inguinal hernias, though secondary to their inguinal / abdominal origin [3].
Hydroceles are most common extra-testicular masses of scrotal origin [4] Epididymal cysts and varicoceles are other extratesticular masses.
Most of the tumours are diagnosed in third and fourth decade of life [5]. Although, no age is exempt of having scrotal masses. Testicular malignant germ cell tumours constitute 90% to 95% of primary tumours. Germ cell tumours are classified as seminomas and non-seminomatous tumours, with seminomas constituting 40% of germ cell tumours. Mixed embryonal cell tumours and terato-carcinomas are the most common non-seminomatous neoplasms, constituting 25% each of germ cell tumours. Other non-seminomatous neoplasms include yolk sac tumours, chorio-carcinomas, teratomas, and various combinations of these cell types.
Scrotal ultrasound is highly accurate modality for differentiating testicular from extra-testicular masses [6]. It determines whether the mass is cystic, solid, or complex [7]. Extensive understanding of ultrasound features of various scrotal masses clearly defines the nature of these masses in experienced hands. MRI shows high signal intensity in malignant cases but is non-specific and is not routinely used. CT examination is performed for staging purposes [8]. Histopathology augments the final diagnosis and helps decide the surgical options – radical surgery for malignant masses whereas testis sparing surgery in benign intra-testicular masses.
[1] Moghe P K, Brady A P. (1999) Ultrasound of testicular epidermoid cysts. The British Journal of Radiology 942-5
[2] Dogra V S, Gottlieb R H, Rubens D J, Liao L. (2001) Benign Intratesticular Cystic Lesions: US Features1. Radiographics S273-81
[3] Ragheb D, Higgins JL Jr. (2002) Ultrasonography of the scrotum: technique, anatomy, and pathologic entities. J Ultra Med 21: 171-85
[4] Iqbal S. (2006) Evaluation of ultrasound diagnosis of scrotal masses using operative findings as gold standard. Dissertation approved by College of Physician & Surgeon of Pakistan 59
[5] Gill M, Shah S, Soomro I, Kayani N, Hasan S (2000) Morphological pattern of testicular tumors. J Pak Med Assoc 50: 110-3
[6] Tahir S. (1997) Tell me the answer, selected questions. Surgery. 3rd ed. Faisalabad: Uro-obs (Pvt) Ltd 660-4
[7] Akin, Khati E A, Hill N J, Michael C. (2004) Ultrasound of the Scrotum. Ultrasound Q 20:181-200
[8] Light D. (2011) Malignant testicular tumor imaging. retrived from: http://emedicine.medscape.com/article/381007-overview
| URL: | https://www.eurorad.org/case/10272 |
| DOI: | 10.1594/EURORAD/CASE.10272 |
| ISSN: | 1563-4086 |