Abdominal ultrasonography
Cholangiocarcinoma: a casual diagnosis in a young man
SectionAbdominal imaging
Case TypeClinical Cases
AuthorsGabelloni M, Fiorini S, Cervelli R, Lorenzoni G, Angeli S, Faggioni L, Bartolozzi C.
Patient39 years, male
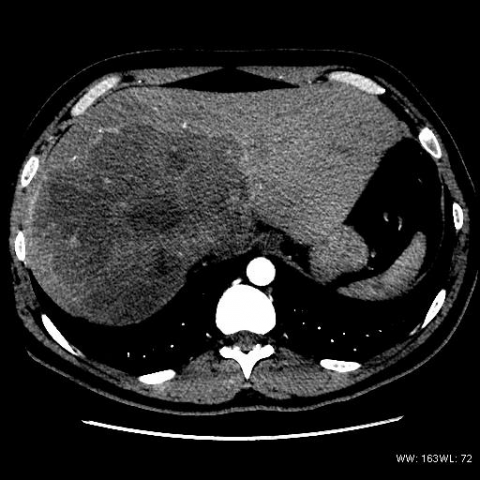
CT findings were indicative of cholangiocarcinoma, mass-forming type. Biopsy of the liver lesion, performed elsewhere, revealed moderately differentiated adenocarcinoma.
A subsequent ultrasound control revealed a satellite nodule in segment IV, along with moderate intrahepatic ductal dilation and gallbladder distention (Fig.4a-c).
Clinical presentation depends on tumour location. Patients with intrahepatic CC often present with dull right upper quadrant discomfort and weight loss, rarely with jaundice. Conversely, patients with extrahepatic CC usually present with painless jaundice, itching, fever, clay-colored stools, and dark urine [1].
CC is classified as either intrahepatic or extrahepatic, and intrahepatic CC is further classified as either peripheral or hilar. A tumour that arises peripherally to the secondary bifurcation of the left or right hepatic duct is considered as peripheral CC, whereas CC arising from the hepatic ducts or the bifurcation of the common hepatic duct is considered as hilar CC (also known as Klatskin tumour).
The Liver Cancer Study Group of Japan has classified intrahepatic cholangiocarcinomas into the mass-forming, periductal infiltrating, and intraductal type. The mass-forming type manifests as a round mass with a distinct border in the liver parenchyma. Periductal infiltrating intrahepatic CC is characterized by tumour infiltration along the bile duct. Finally, intraductal intrahepatic CC is characterized by papillary or granular growth within the bile duct lumen [2-5].
Ultrasound is the first-level imaging modality for diagnosis and has high sensitivity for visualizing the bile ducts, confirming ductal dilatation, and ruling out choledocholithiasis.
Contrast-enhanced multidetector computed tomography (MDCT) is usually performed as a second-level imaging examination to confirm the diagnosis of CC and perform disease staging. Triple-phase helical CT has a sensitivity near 100% in detecting CC larger than 1cm, allows detection of nodal metastases and distant disease dissemination, and can provide detailed information on vascular anatomy that is useful for surgical planning.
Magnetic resonance cholangiopancreatography (MRCP) has the capability to evaluate the bile ducts both above and below the lesion, and can also directly identify intrahepatic mass lesions.
Invasive cholangiography may provide diagnostic data in the form of brush cytology and may be required preoperatively for therapeutic biliary drainage. It can be performed by endoscopic retrograde cholangiopancreatography (ERCP) or by a percutaneous transhepatic cholangiography (PTC).
Surgery remains the only curative treatment. Chemotherapy is currently unable to significantly improve survival in patients with either resected or unresected CC. Most patients with an unresectable tumour die between 6 months and 1 year following diagnosis [1].
[1] Anderson CD, Pinson W, Berlin J, Chari RS (2004) Diagnosis and treatment of cholangiocarcinoma. The oncologist 9: 43-57 (PMID: 14755014)
[2] Han K, Choi BI, Kim AY, An SK, Lee W, Kim TK, Kim SW (2002) Cholangiocarcinoma: pictorial essay of CT and cholangiographic findings. Radiographics 22: 173-187 (PMID: 11796906)
[3] Sainani NI, Catalano OA, Holalkere NS, Zhu AX, Hahn PF, Sahani DV. (2008) Cholangiocarcinoma: current and novel imaging techniques. Radiographics 28:1263-1287 (PMID: 18794305)
[4] Chung YE, Kim MJ, Park YN, Choi JY, Pyo JY, Kim YC, Cho HJ, Kim KA, Choi SY. (2009) Varying appearances of cholangiocarcinoma: radiologic-pathologic correlation. Radiographics 29:683-700 (PMID: 19448110)
[5] Menias CO, Surabhi VR, Prasad SR, Wang HL, Narra VR, Chintapalli KN. (2008) Mimics of cholangiocarcinoma: spectrum of disease. Radiographics 28:1115-1129 (PMID: 18635632)
| URL: | https://www.eurorad.org/case/10485 |
| DOI: | 10.1594/EURORAD/CASE.10485 |
| ISSN: | 1563-4086 |